Are you gearing up for a career shift or aiming to ace your next interview? Look no further! We’ve curated a comprehensive guide to help you crack the interview for the coveted Medicaid Analyst position. From understanding the key responsibilities to mastering the most commonly asked questions, this blog has you covered. So, buckle up and let’s embark on this journey together.
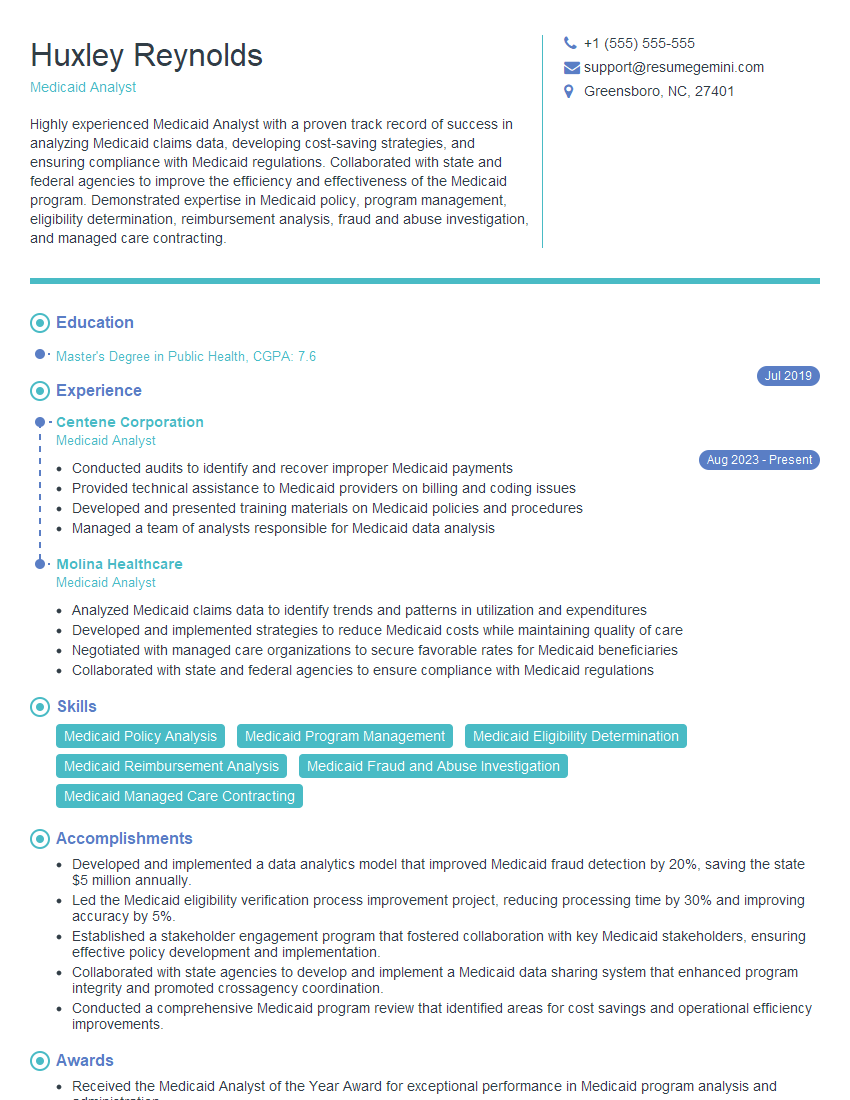
Acing the interview is crucial, but landing one requires a compelling resume that gets you noticed. Crafting a professional document that highlights your skills and experience is the first step toward interview success. ResumeGemini can help you build a standout resume that gets you called in for that dream job.
Essential Interview Questions For Medicaid Analyst
1. What are the primary responsibilities of a Medicaid Analyst?
As a Medicaid Analyst, my key responsibilities would include:
- Analyzing Medicaid data to identify trends, patterns, and areas for improvement.
- Developing and implementing strategies to improve the efficiency and effectiveness of Medicaid programs.
- Collaborating with stakeholders, including healthcare providers, policymakers, and beneficiaries, to gather input and ensure alignment.
2. Describe your experience in analyzing Medicaid data.
Data Analysis Techniques
- Proficient in statistical analysis techniques, such as regression analysis, ANOVA, and data mining.
- Familiar with software tools for data analysis, such as SAS, SPSS, and R.
Applications
- Analyzed Medicaid claims data to identify high-cost providers and utilization patterns.
- Developed predictive models to forecast future Medicaid expenditures.
- Used data visualization tools to present findings in a clear and concise manner.
3. How do you approach developing and implementing strategies to improve Medicaid programs?
My approach involves:
- Conducting a thorough needs assessment to identify areas for improvement.
- Engaging stakeholders to co-create and prioritize solutions.
- Developing evidence-based strategies informed by data analysis.
- Implementing the strategies in a phased manner with regular monitoring and evaluation.
4. What challenges have you encountered in your previous role as a Medicaid Analyst? How did you overcome them?
In my previous role, I encountered challenges such as:
- Data quality issues: I addressed this by implementing data cleaning and validation procedures.
- Stakeholder engagement: I overcame this by actively seeking out stakeholder input and building relationships.
- Resource constraints: I prioritized tasks and sought support from colleagues to efficiently manage my workload.
5. How do you stay up-to-date on the latest Medicaid policies and regulations?
- Regularly reviewing government publications and websites.
- Attending industry conferences and webinars.
- Networking with other Medicaid professionals.
6. What are the key ethical considerations in Medicaid data analysis?
- Confidentiality: Ensuring the privacy and security of beneficiary information.
- Equity: Analyzing data to identify and address disparities in access and outcomes.
- Transparency: Clear and open communication of data analysis findings.
7. How do you handle situations where your analysis leads to recommendations that may not be popular with stakeholders?
- Present the findings objectively: Focus on the data and evidence without bias.
- Engage stakeholders in dialogue: Facilitate an open discussion about the implications and potential solutions.
- Seek compromise: Work with stakeholders to identify solutions that balance different perspectives.
8. What is your experience with Medicaid reimbursement methodologies?
- Fee-for-service: Analyzed claims data to assess provider payments and identify opportunities for cost savings.
- Managed care: Evaluated capitation rates and performance-based payments.
- Value-based purchasing: Developed metrics to measure provider quality and incentivize improved outcomes.
9. How do you evaluate the effectiveness of Medicaid interventions?
- Establish clear objectives: Define what the intervention is intended to achieve.
- Collect baseline data: Gather data before the intervention to provide a comparison point.
- Implement the intervention and monitor progress: Track key metrics to assess impact.
- Evaluate outcomes: Analyze the data to determine whether the desired outcomes were achieved.
10. What are your strengths and weaknesses as a Medicaid Analyst?
Strengths:
- Strong analytical skills and data interpretation abilities.
- Excellent communication and stakeholder engagement skills.
- Deep understanding of Medicaid policies and regulations.
Weaknesses:
- Limited experience with certain Medicaid populations (e.g., behavioral health).
- Could improve time management skills in high-pressure situations.
Interviewers often ask about specific skills and experiences. With ResumeGemini‘s customizable templates, you can tailor your resume to showcase the skills most relevant to the position, making a powerful first impression. Also check out Resume Template specially tailored for Medicaid Analyst.
Career Expert Tips:
- Ace those interviews! Prepare effectively by reviewing the Top 50 Most Common Interview Questions on ResumeGemini.
- Navigate your job search with confidence! Explore a wide range of Career Tips on ResumeGemini. Learn about common challenges and recommendations to overcome them.
- Craft the perfect resume! Master the Art of Resume Writing with ResumeGemini’s guide. Showcase your unique qualifications and achievements effectively.
- Great Savings With New Year Deals and Discounts! In 2025, boost your job search and build your dream resume with ResumeGemini’s ATS optimized templates.
Researching the company and tailoring your answers is essential. Once you have a clear understanding of the Medicaid Analyst‘s requirements, you can use ResumeGemini to adjust your resume to perfectly match the job description.
Key Job Responsibilities
Medicaid Analysts play a vital role in the healthcare industry, ensuring that Medicaid programs are running efficiently and effectively.
1. Analyze Medicaid Data
Medicaid Analysts collect and analyze data from various sources to identify trends, patterns, and areas for improvement within Medicaid programs.
- Assess claims data to identify errors or fraud.
- Evaluate program utilization to determine if services are being delivered in an effective and equitable manner.
2. Develop and Implement Policy Recommendations
Based on their analysis, Medicaid Analysts develop and implement policy recommendations to improve the efficiency, effectiveness, and equity of Medicaid programs.
- Propose changes to Medicaid regulations or policies to improve program outcomes.
- Conduct cost-benefit analyses to evaluate the potential impact of proposed policy changes.
3. Monitor and Evaluate Medicaid Programs
Medicaid Analysts monitor and evaluate the implementation of Medicaid programs to ensure they are meeting their objectives and targets.
- Track progress towards program goals and objectives.
- Identify areas where programs can be improved or streamlined.
4. Provide Technical Assistance
Medicaid Analysts provide technical assistance to healthcare providers, state agencies, and other stakeholders on Medicaid program policies and procedures.
- Conduct training and workshops to educate stakeholders on Medicaid program requirements.
- Answer questions and provide guidance on Medicaid program implementation.
Interview Tips
Preparing for a Medicaid Analyst interview requires a combination of technical knowledge and soft skills. Here are some tips to help you ace the interview:
1. Research the Organization and Position
Take the time to thoroughly research the organization you’re applying to and the specific position you’re interested in. This will help you understand the company’s culture, goals, and specific needs for the role.
- Review the organization’s website, annual reports, and social media presence.
- Identify the key responsibilities and qualifications for the Medicaid Analyst position.
2. Highlight Your Skills and Experience
In your resume and cover letter, be sure to highlight your skills and experience that are relevant to the Medicaid Analyst role. Quantify your accomplishments whenever possible to demonstrate your impact.
- Emphasize your experience in data analysis, policy development, or program evaluation.
- Provide examples of how you have successfully improved the efficiency or effectiveness of healthcare programs.
3. Prepare for Common Interview Questions
There are certain interview questions that are commonly asked in Medicaid Analyst interviews. Prepare for these questions by practicing your answers and thinking about specific examples from your experience.
- Tell me about your experience in analyzing Medicaid data.
- What is your understanding of Medicaid policy and regulations?
- How would you approach developing policy recommendations to improve a Medicaid program?
- What is your experience in providing technical assistance to healthcare providers?
4. Ask Thoughtful Questions
Asking thoughtful questions at the end of the interview shows that you are engaged and interested in the position. It also gives you an opportunity to learn more about the organization and the role.
- Ask about the organization’s strategic priorities and how the Medicaid Analyst role contributes to those goals.
- Inquire about the challenges and opportunities facing the Medicaid program in the current healthcare environment.
Next Step:
Now that you’re armed with interview-winning answers and a deeper understanding of the Medicaid Analyst role, it’s time to take action! Does your resume accurately reflect your skills and experience for this position? If not, head over to ResumeGemini. Here, you’ll find all the tools and tips to craft a resume that gets noticed. Don’t let a weak resume hold you back from landing your dream job. Polish your resume, hit the “Build Your Resume” button, and watch your career take off! Remember, preparation is key, and ResumeGemini is your partner in interview success.