Are you a seasoned Benefit Authorizer seeking a new career path? Discover our professionally built Benefit Authorizer Resume Template. This time-saving tool provides a solid foundation for your job search. Simply click “Edit Resume” to customize it with your unique experiences and achievements. Customize fonts and colors to match your personal style and increase your chances of landing your dream job. Explore more Resume Templates for additional options.
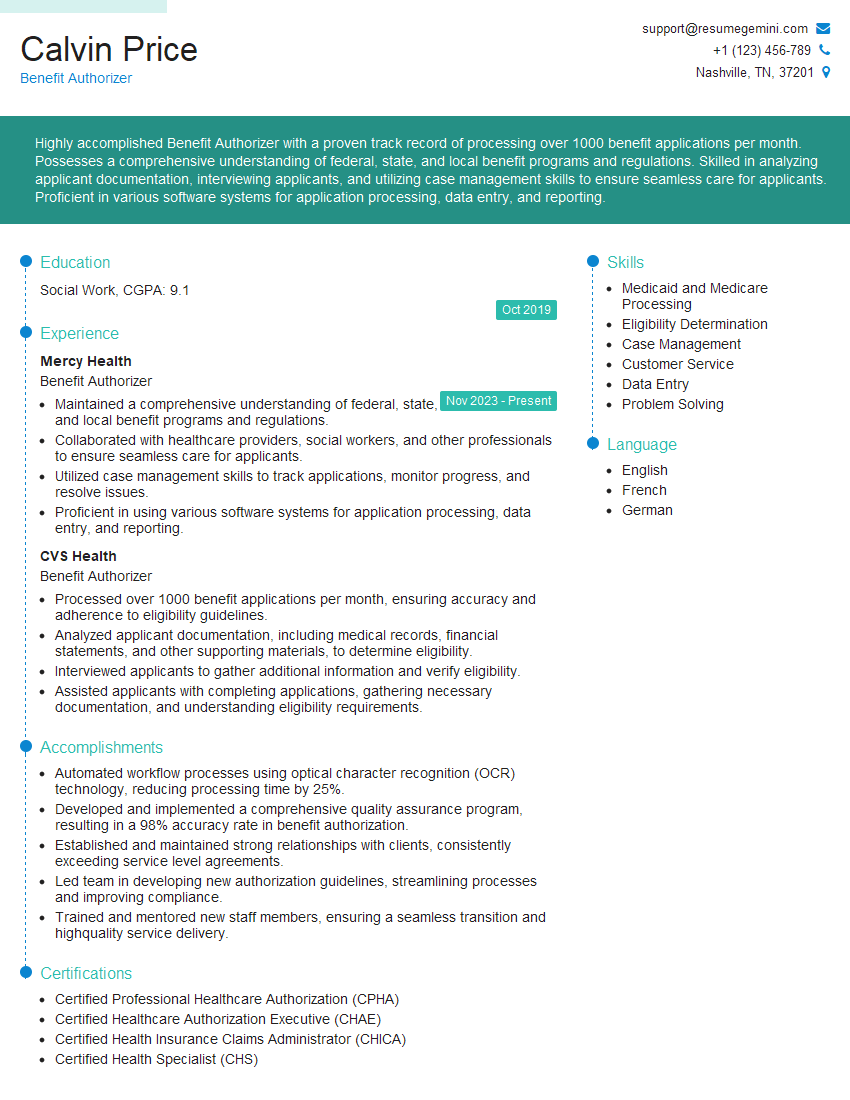
Calvin Price
Benefit Authorizer
Summary
Highly accomplished Benefit Authorizer with a proven track record of processing over 1000 benefit applications per month. Possesses a comprehensive understanding of federal, state, and local benefit programs and regulations. Skilled in analyzing applicant documentation, interviewing applicants, and utilizing case management skills to ensure seamless care for applicants. Proficient in various software systems for application processing, data entry, and reporting.
Education
Social Work
October 2019
Skills
- Medicaid and Medicare Processing
- Eligibility Determination
- Case Management
- Customer Service
- Data Entry
- Problem Solving
Work Experience
Benefit Authorizer
- Maintained a comprehensive understanding of federal, state, and local benefit programs and regulations.
- Collaborated with healthcare providers, social workers, and other professionals to ensure seamless care for applicants.
- Utilized case management skills to track applications, monitor progress, and resolve issues.
- Proficient in using various software systems for application processing, data entry, and reporting.
Benefit Authorizer
- Processed over 1000 benefit applications per month, ensuring accuracy and adherence to eligibility guidelines.
- Analyzed applicant documentation, including medical records, financial statements, and other supporting materials, to determine eligibility.
- Interviewed applicants to gather additional information and verify eligibility.
- Assisted applicants with completing applications, gathering necessary documentation, and understanding eligibility requirements.
Accomplishments
- Automated workflow processes using optical character recognition (OCR) technology, reducing processing time by 25%.
- Developed and implemented a comprehensive quality assurance program, resulting in a 98% accuracy rate in benefit authorization.
- Established and maintained strong relationships with clients, consistently exceeding service level agreements.
- Led team in developing new authorization guidelines, streamlining processes and improving compliance.
- Trained and mentored new staff members, ensuring a seamless transition and highquality service delivery.
Certificates
- Certified Professional Healthcare Authorization (CPHA)
- Certified Healthcare Authorization Executive (CHAE)
- Certified Health Insurance Claims Administrator (CHICA)
- Certified Health Specialist (CHS)
Languages
- English
- French
- German
Career Expert Tips:
- Select the ideal resume template to showcase your professional experience effectively.
- Master the art of resume writing to highlight your unique qualifications and achievements.
- Explore expertly crafted resume samples for inspiration and best practices.
- Build your best resume for free this new year with ResumeGemini. Enjoy exclusive discounts on ATS optimized resume templates.
How To Write Resume For Benefit Authorizer
- Highlight your experience in processing a high volume of applications accurately and efficiently.
- Emphasize your knowledge of federal, state, and local benefit programs and regulations.
- Showcase your skills in analyzing complex documentation and interviewing applicants to determine eligibility.
- Demonstrate your ability to provide excellent customer service and assist applicants with completing applications and gathering necessary documentation.
- Include quantifiable results, such as the number of applications processed or the percentage of applications approved.
Essential Experience Highlights for a Strong Benefit Authorizer Resume
- Processed over 1000 benefit applications per month, ensuring accuracy and adherence to eligibility guidelines.
- Analyzed applicant documentation, including medical records, financial statements, and other supporting materials, to determine eligibility.
- Interviewed applicants to gather additional information and verify eligibility.
- Assisted applicants with completing applications, gathering necessary documentation, and understanding eligibility requirements.
- Maintained a comprehensive understanding of federal, state, and local benefit programs and regulations.
- Collaborated with healthcare providers, social workers, and other professionals to ensure seamless care for applicants.
- Utilized case management skills to track applications, monitor progress, and resolve issues.
- Proficient in using various software systems for application processing, data entry, and reporting.
Frequently Asked Questions (FAQ’s) For Benefit Authorizer
What are the key responsibilities of a Benefit Authorizer?
The key responsibilities of a Benefit Authorizer include processing benefit applications, analyzing applicant documentation, interviewing applicants, assisting applicants with completing applications and understanding eligibility requirements, maintaining a comprehensive understanding of federal, state, and local benefit programs and regulations, collaborating with healthcare providers, social workers, and other professionals to ensure seamless care for applicants, and utilizing case management skills to track applications, monitor progress, and resolve issues.
What are the qualifications for a Benefit Authorizer?
The qualifications for a Benefit Authorizer typically include a high school diploma or equivalent, experience in processing benefits applications, knowledge of federal, state, and local benefit programs and regulations, and excellent customer service skills.
What is the job outlook for Benefit Authorizers?
The job outlook for Benefit Authorizers is expected to grow faster than average in the coming years due to the increasing demand for healthcare and social services.
What are the salary expectations for Benefit Authorizers?
The salary expectations for Benefit Authorizers vary depending on experience, location, and employer. According to Salary.com, the average salary for a Benefit Authorizer is around $45,000 per year.
What are the benefits of working as a Benefit Authorizer?
The benefits of working as a Benefit Authorizer can include a competitive salary, health insurance, paid time off, and the opportunity to make a difference in the lives of others.
What are the challenges of working as a Benefit Authorizer?
The challenges of working as a Benefit Authorizer can include the high volume of applications to process, the need to stay up-to-date on federal, state, and local benefit programs and regulations, and the potential for dealing with difficult applicants.