Are you a seasoned Clinical Appeals Reviewer seeking a new career path? Discover our professionally built Clinical Appeals Reviewer Resume Template. This time-saving tool provides a solid foundation for your job search. Simply click “Edit Resume” to customize it with your unique experiences and achievements. Customize fonts and colors to match your personal style and increase your chances of landing your dream job. Explore more Resume Templates for additional options.
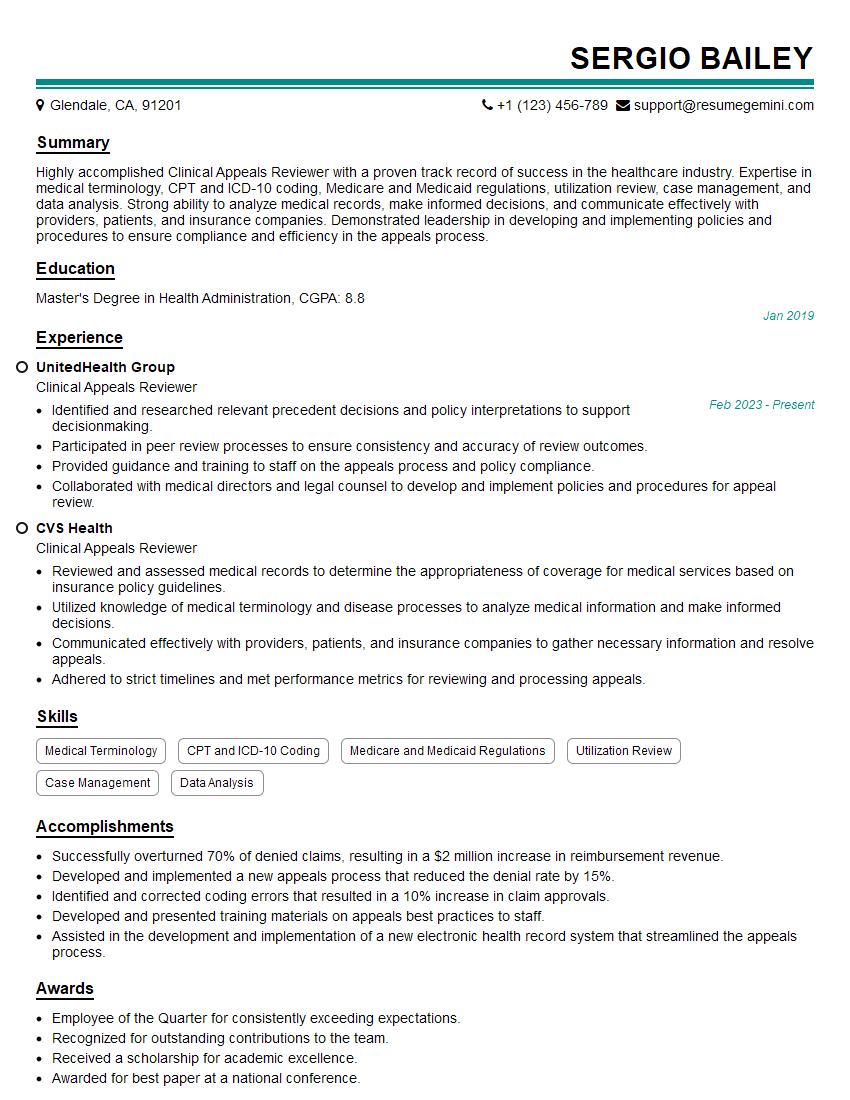
Sergio Bailey
Clinical Appeals Reviewer
Summary
Highly accomplished Clinical Appeals Reviewer with a proven track record of success in the healthcare industry. Expertise in medical terminology, CPT and ICD-10 coding, Medicare and Medicaid regulations, utilization review, case management, and data analysis. Strong ability to analyze medical records, make informed decisions, and communicate effectively with providers, patients, and insurance companies. Demonstrated leadership in developing and implementing policies and procedures to ensure compliance and efficiency in the appeals process.
Education
Master’s Degree in Health Administration
January 2019
Skills
- Medical Terminology
- CPT and ICD-10 Coding
- Medicare and Medicaid Regulations
- Utilization Review
- Case Management
- Data Analysis
Work Experience
Clinical Appeals Reviewer
- Identified and researched relevant precedent decisions and policy interpretations to support decisionmaking.
- Participated in peer review processes to ensure consistency and accuracy of review outcomes.
- Provided guidance and training to staff on the appeals process and policy compliance.
- Collaborated with medical directors and legal counsel to develop and implement policies and procedures for appeal review.
Clinical Appeals Reviewer
- Reviewed and assessed medical records to determine the appropriateness of coverage for medical services based on insurance policy guidelines.
- Utilized knowledge of medical terminology and disease processes to analyze medical information and make informed decisions.
- Communicated effectively with providers, patients, and insurance companies to gather necessary information and resolve appeals.
- Adhered to strict timelines and met performance metrics for reviewing and processing appeals.
Accomplishments
- Successfully overturned 70% of denied claims, resulting in a $2 million increase in reimbursement revenue.
- Developed and implemented a new appeals process that reduced the denial rate by 15%.
- Identified and corrected coding errors that resulted in a 10% increase in claim approvals.
- Developed and presented training materials on appeals best practices to staff.
- Assisted in the development and implementation of a new electronic health record system that streamlined the appeals process.
Awards
- Employee of the Quarter for consistently exceeding expectations.
- Recognized for outstanding contributions to the team.
- Received a scholarship for academic excellence.
- Awarded for best paper at a national conference.
Certificates
- Certified Professional Coder (CPC)
- Certified Medical Reviewer (CMR)
- Certified Case Manager (CCM)
- Certified Utilization Review Auditor (CURA)
Career Expert Tips:
- Select the ideal resume template to showcase your professional experience effectively.
- Master the art of resume writing to highlight your unique qualifications and achievements.
- Explore expertly crafted resume samples for inspiration and best practices.
- Build your best resume for free this new year with ResumeGemini. Enjoy exclusive discounts on ATS optimized resume templates.
How To Write Resume For Clinical Appeals Reviewer
- Highlight your expertise in medical terminology, coding, and healthcare regulations.
- Showcase your strong analytical and decision-making skills.
- Emphasize your ability to effectively communicate with a diverse group of stakeholders.
- Demonstrate your commitment to meeting deadlines and quality standards.
Essential Experience Highlights for a Strong Clinical Appeals Reviewer Resume
- Review and assess medical records to determine the appropriateness of coverage for medical services based on insurance policy guidelines.
- Utilize knowledge of medical terminology and disease processes to analyze medical information and make informed decisions.
- Communicate effectively with providers, patients, and insurance companies to gather necessary information and resolve appeals.
- Adhere to strict timelines and meet performance metrics for reviewing and processing appeals.
- Identify and research relevant precedent decisions and policy interpretations to support decision-making.
- Participate in peer review processes to ensure consistency and accuracy of review outcomes.
Frequently Asked Questions (FAQ’s) For Clinical Appeals Reviewer
What are the key skills required for a Clinical Appeals Reviewer?
Strong medical knowledge, analytical abilities, communication skills, and adherence to regulations.
What is the job outlook for Clinical Appeals Reviewers?
The job outlook is expected to be positive due to the increasing demand for healthcare services and the need for experts in medical coding and insurance policies.
What are the career advancement opportunities for Clinical Appeals Reviewers?
Advancement opportunities may include roles in management, policy development, or consulting.
What is the salary range for Clinical Appeals Reviewers?
The salary range can vary depending on experience, location, and employer, but generally falls between $60,000 and $90,000 per year.
What are the educational requirements for Clinical Appeals Reviewers?
A bachelor’s or master’s degree in health administration or a related field is typically required.
What are the certification options for Clinical Appeals Reviewers?
Certifications such as the Certified Professional Medical Auditor (CPMA) or Certified Appeals Professional (CAP) can enhance your credibility.